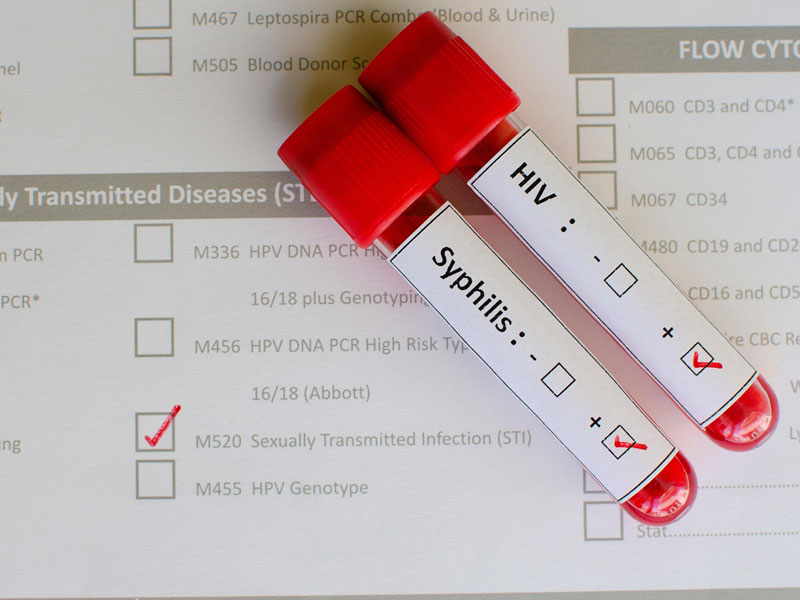
Sexually transmitted infections (STIs) are often diagnosed through laboratory testing, including blood tests. Different infections require different testing methods. Some STIs are readily detectable through blood work, while others may require specialized tests like urine samples or swabs. For instance, syphilis and HIV are typically diagnosed through blood tests. Other infections, like chlamydia or gonorrhea, are usually diagnosed using samples collected from the affected area.
Early detection of STIs is crucial for effective treatment and preventing long-term health complications. Blood tests offer a convenient and reliable method for diagnosing certain infections, allowing healthcare professionals to initiate appropriate treatment promptly. The development of reliable blood tests has significantly improved STI management and public health outcomes. Historical context reveals a shift from less sensitive diagnostic methods to more accurate and efficient blood-based assays.
This discussion underscores the importance of regular STI screening and the role of blood tests in diagnosis. The following sections will delve into specific STIs, their respective diagnostic methods, and available treatment options.
1. STI Type
The type of sexually transmitted infection (STI) significantly influences its detectability through blood work. Certain STIs, such as HIV and syphilis, produce antibodies or antigens readily identifiable in blood serum. These infections are routinely diagnosed using blood tests like enzyme-linked immunosorbent assays (ELISAs) or rapid plasma reagin (RPR) tests. Conversely, infections like chlamydia and gonorrhea primarily reside in mucosal tissues, making them less reliably detected through standard blood tests. Nucleic acid amplification tests (NAATs) on urine samples or swabs from the affected area offer greater sensitivity for diagnosing these infections. Herpes simplex virus (HSV) can be detected through blood tests, although viral culture or polymerase chain reaction (PCR) testing of lesion swabs are sometimes preferred for confirmation. Thus, the choice of diagnostic test depends heavily on the suspected STI.
Understanding this connection between STI type and appropriate diagnostic methods is crucial for effective healthcare. For instance, relying solely on blood tests to screen for all STIs could lead to false negatives for infections like chlamydia, potentially delaying treatment and increasing the risk of transmission. Conversely, utilizing more invasive procedures when a simple blood test would suffice is unnecessary. Clinicians must consider the patient’s symptoms, sexual history, and the prevalence of different STIs in the population when selecting the most appropriate diagnostic strategy. Furthermore, recognizing which STIs are readily detectable through routine blood work can inform public health screening programs and resource allocation.
In summary, the relationship between STI type and diagnostic method is complex and requires careful consideration. Employing the correct testing strategy, based on the suspected STI, maximizes diagnostic accuracy and facilitates timely intervention. This understanding is essential for effective individual patient management and broader public health initiatives aimed at controlling STI transmission. The challenges lie in ensuring access to appropriate testing and educating both patients and healthcare providers about the nuances of STI diagnosis.
2. Testing Methods
Determining whether sexually transmitted infections (STIs) are detectable through blood work hinges critically on the employed testing methods. Different STIs exhibit varying characteristics, necessitating specific laboratory techniques for accurate detection. Selecting the appropriate method is crucial for reliable diagnosis and subsequent treatment strategies.
-
Serological Tests
Serological tests identify antibodies or antigens produced by the body in response to an infection. Enzyme-linked immunosorbent assays (ELISAs) and chemiluminescence immunoassays (CLIAs) are commonly used to detect antibodies against HIV, syphilis, and hepatitis B. Rapid plasma reagin (RPR) tests detect antibodies indicative of syphilis. While serological tests are valuable for detecting past or current infections, they may not be reliable during the initial stages of infection when antibody levels are still low.
-
Nucleic Acid Amplification Tests (NAATs)
NAATs detect the genetic material (DNA or RNA) of the infectious agent. These tests offer high sensitivity and specificity, particularly for infections like chlamydia and gonorrhea, which are not reliably detected through blood tests. NAATs are typically performed on urine samples, swabs from the affected area, or sometimes blood. They are essential for diagnosing infections in early stages and can also be used to monitor treatment response.
-
Culture Tests
Culture tests involve growing the infectious agent in a laboratory setting. This method is often used to diagnose infections like gonorrhea, chlamydia, and herpes. While highly specific, culture tests can be time-consuming and require specialized laboratory facilities. Their use is generally limited to specific clinical scenarios or when other diagnostic methods are inconclusive.
-
Microscopy
Microscopic examination of tissue samples or fluids can sometimes identify the presence of infectious agents. For example, the detection of Trichomonas vaginalis, a parasite causing trichomoniasis, can be achieved through microscopic analysis of vaginal discharge. This method is generally less sensitive than NAATs or culture tests but can provide rapid, preliminary diagnostic information in certain cases.
The effectiveness of STI detection through blood work depends directly on the testing method employed. While blood tests are valuable for certain infections, others require specialized techniques like NAATs, cultures, or microscopy. Understanding the strengths and limitations of each method allows clinicians to select the most appropriate approach, ensuring accurate diagnosis and informing effective treatment strategies. Ultimately, the choice of testing method must be tailored to the specific suspected infection and the individual clinical circumstances.
3. Detection Window
The “detection window” refers to the period between initial infection with a sexually transmitted infection (STI) and the point when the infection becomes detectable through testing. This period varies significantly depending on the specific STI and the testing method employed. Understanding the detection window is crucial for interpreting test results accurately and ensuring timely diagnosis and treatment. It directly impacts whether an STI will show up in blood work or other diagnostic tests at a given time.
-
Window Period Variability
Different STIs have distinct window periods. For example, HIV antibodies typically become detectable within a few weeks of infection, while it can take several months for syphilis antibodies to reach detectable levels. This variability underscores the importance of considering the specific suspected STI and its associated detection window when interpreting test results. A negative result obtained before the end of the detection window may not definitively rule out infection, necessitating repeat testing at a later date.
-
Testing Method Influence
The chosen testing method also influences the detection window. Nucleic acid amplification tests (NAATs), which detect the genetic material of the pathogen, generally have shorter detection windows compared to antibody-based tests. For instance, NAATs can detect chlamydia and gonorrhea infections sooner than serological tests. This difference highlights the importance of selecting the appropriate testing method based on the suspected STI and the time elapsed since potential exposure.
-
Implications for Diagnosis
The detection window has significant implications for diagnosis. A negative test result obtained within the detection window may provide false reassurance, potentially delaying diagnosis and treatment. This delay can have serious consequences, particularly for infections that can cause long-term health complications if left untreated. Furthermore, it increases the risk of onward transmission to others. Understanding the detection window is therefore crucial for interpreting test results accurately and making informed decisions about further testing and treatment.
-
Impact on Public Health
The concept of the detection window is also relevant to public health efforts. Accurate estimates of STI prevalence within a population rely on reliable testing data. Failure to account for the detection window can lead to underestimation of true infection rates, as some individuals may be infected but not yet detectable through testing. This information is crucial for designing effective prevention and intervention programs.
In conclusion, the detection window is a critical factor in interpreting STI test results, especially those obtained through blood work. The variability of detection windows across different STIs and testing methods necessitates a nuanced understanding of these factors. Accurate interpretation of test results and informed decision-making about further testing, treatment, and public health interventions rely heavily on considering the detection window. Ignoring this crucial aspect can lead to delayed diagnosis, ongoing transmission, and inaccurate estimations of disease prevalence.
4. Accuracy Variations
Accuracy variations in STI testing are inherent and understanding these nuances is paramount when interpreting results, particularly concerning blood work. While laboratory diagnostics strive for precision, various factors can influence test outcomes. These variations directly impact the reliability of determining whether STIs manifest in blood work, impacting both diagnosis and subsequent treatment strategies.
-
Biological Factors
Biological factors within the individual being tested can influence accuracy. The stage of infection plays a critical role; during the initial “window period,” antibody levels might be too low for detection, leading to false negatives. Individual immune responses also vary, impacting antibody production and detectability. Co-existing conditions, such as other infections or autoimmune disorders, can potentially interfere with test accuracy.
-
Test Characteristics
Each test possesses inherent limitations. Sensitivity, the ability to correctly identify infected individuals, and specificity, the ability to correctly identify uninfected individuals, contribute to potential variations. No test achieves perfect sensitivity and specificity. False negatives can occur with low sensitivity, while low specificity can yield false positives. Understanding these test characteristics is crucial for result interpretation.
-
Laboratory Procedures
Variations in laboratory procedures can influence results. Proper sample collection, handling, and storage are essential for accurate analysis. Variations in equipment calibration, reagent quality, or technician proficiency can introduce errors. Quality control measures within laboratories are critical for minimizing these variations and ensuring reliable results.
-
Human Error
Despite standardized protocols, human error can introduce variability. Mistakes in sample labeling, data entry, or result interpretation can lead to inaccuracies. Implementing robust quality assurance systems, including double-checking procedures and staff training, helps mitigate these risks.
These accuracy variations underscore the complexity of interpreting STI test results, especially concerning blood work. While blood tests provide valuable diagnostic information for certain STIs, recognizing the potential for variations is crucial. Clinicians must consider these factors alongside patient history, symptoms, and other clinical findings to reach accurate diagnoses. Furthermore, open communication between healthcare providers and patients about the potential for variations is essential for informed decision-making regarding treatment and prevention strategies.
5. False Negatives
False negatives in STI testing, particularly concerning blood work, pose a significant challenge to accurate diagnosis and disease management. A false negative occurs when a test incorrectly indicates the absence of an infection when, in fact, the individual is infected. This discrepancy can arise from various factors, impacting the reliability of determining whether STIs manifest in blood work and potentially leading to delayed treatment and continued transmission.
Several factors contribute to false negatives. The “window period” the time between infection and detectable antibody or antigen levels plays a crucial role. Testing too early in the course of infection can yield a false negative result, even if the individual is infected. Certain STIs, like chlamydia and gonorrhea, are not reliably detected through blood work, necessitating more specific tests like nucleic acid amplification tests (NAATs) performed on urine or swabs. Relying solely on blood tests for these infections increases the risk of false negatives. Test sensitivity, the ability of a test to correctly identify infected individuals, also influences accuracy. No test is perfectly sensitive, and variations in test performance can contribute to false negatives. Laboratory errors, such as improper sample handling or technical issues, can also lead to inaccurate results. Furthermore, individual biological factors, like a compromised immune system, can affect antibody production and impact test accuracy.
The consequences of false negatives are substantial. Delayed diagnosis and treatment can lead to further disease progression and increase the risk of long-term health complications, including infertility and chronic pain. False negatives can also facilitate ongoing transmission within the population, as individuals unaware of their infection may unknowingly expose others. Addressing the challenge of false negatives requires a multi-faceted approach. Clinicians must carefully consider the detection window for each STI and select appropriate testing methods based on the individual’s risk factors and symptoms. Repeat testing might be necessary, especially if initial results are negative and clinical suspicion remains high. Public health efforts aimed at increasing awareness about STI testing and promoting early diagnosis are essential for mitigating the impact of false negatives on individual and community health. Further research into improving test accuracy and developing more sensitive diagnostic tools is also crucial for reducing the incidence of false negatives and enhancing STI control efforts.
6. Confirmatory Testing
Confirmatory testing plays a critical role in accurately diagnosing sexually transmitted infections (STIs), especially when initial screening results, including those from blood work, are positive or inconclusive. It provides a higher level of certainty, reducing the likelihood of false positives and ensuring appropriate treatment decisions. The need for confirmatory testing hinges on the limitations of initial screening tests and the potential impact of misdiagnosis.
-
Ensuring Diagnostic Accuracy
Initial screening tests, while valuable for identifying potential infections, may not always be definitive. Biological factors, test limitations, or laboratory variations can contribute to false-positive results. Confirmatory testing utilizes different methodologies with higher specificity to validate initial reactive results, reducing diagnostic uncertainty. This is particularly crucial for STIs with significant health implications, such as HIV or syphilis, where accurate diagnosis is essential for timely intervention.
-
Guiding Treatment Decisions
Accurate diagnosis is fundamental for guiding treatment decisions. Initiating treatment based on a false-positive result exposes individuals to unnecessary medication with potential side effects, while a false negative delays essential treatment. Confirmatory testing provides the necessary validation to ensure treatment is administered only when genuinely required, optimizing patient care and resource allocation.
-
Addressing Public Health Concerns
Confirmatory testing contributes significantly to accurate surveillance data. Reliable diagnostic information is essential for understanding STI prevalence, identifying at-risk populations, and designing effective public health interventions. By minimizing diagnostic errors, confirmatory testing improves the quality of epidemiological data, informing evidence-based prevention strategies and resource allocation.
-
Specific STI Examples
The approach to confirmatory testing varies depending on the specific STI. For example, a positive initial HIV antibody test might be followed by a Western blot or a different antibody differentiation assay. A reactive RPR test for syphilis typically requires confirmation with a treponemal test like Treponema pallidum particle agglutination (TP-PA). These specific confirmatory tests provide a higher level of certainty, minimizing the risk of misdiagnosis and ensuring appropriate management.
Confirmatory testing provides a crucial layer of validation in STI diagnosis, particularly when initial blood work or other screening tests yield positive or ambiguous results. By reducing diagnostic uncertainty, confirmatory testing ensures appropriate treatment decisions, strengthens public health surveillance efforts, and ultimately improves patient care and disease management. Its importance underscores the complexity of STI diagnosis and the need for a comprehensive approach that incorporates multiple testing strategies to achieve accurate and reliable results.
Frequently Asked Questions About STI Blood Tests
This section addresses common queries regarding the detection of sexually transmitted infections (STIs) through blood work, offering clear and concise information to promote understanding and informed decision-making.
Question 1: Are all STIs detectable through blood tests?
No. While blood tests effectively detect certain STIs like HIV and syphilis, others, such as chlamydia and gonorrhea, require specialized tests like nucleic acid amplification tests (NAATs) on urine or swabs from the affected area. The appropriate testing method depends on the specific STI.
Question 2: How soon after potential exposure can an STI be detected through blood work?
The detection window, the time between infection and detectability, varies depending on the STI and the testing method. For some infections, antibodies or antigens may not be detectable for several weeks or even months after exposure. Consulting a healthcare professional regarding appropriate testing timelines based on individual circumstances is crucial.
Question 3: Can blood tests definitively rule out an STI?
A negative blood test result does not always definitively rule out an infection, especially if testing occurs within the detection window. False negatives can occur. If symptoms persist or concerns remain, repeat testing might be necessary. Open communication with a healthcare provider is crucial for proper interpretation of test results.
Question 4: Are blood tests for STIs always accurate?
While blood tests are generally accurate, variations can occur due to biological factors, test limitations, or laboratory procedures. False positives and false negatives are possible. Confirmatory testing is often necessary to validate initial reactive results and ensure accurate diagnosis.
Question 5: What should someone do if they receive a positive STI test result from blood work?
Individuals receiving a positive result should consult a healthcare professional promptly for further evaluation and appropriate management. Confirmatory testing might be necessary to validate the initial result. Timely medical intervention is crucial for effective treatment and preventing potential complications.
Question 6: How can one ensure accurate STI testing results?
Accurate testing relies on several factors. Open communication with a healthcare provider about sexual history and potential exposures is essential. Selecting the appropriate testing method based on the suspected STI is crucial. Adhering to recommended testing timelines and following up on results with a healthcare professional are key steps in ensuring accurate diagnosis and appropriate management.
Understanding the limitations and benefits of STI blood tests empowers individuals to make informed decisions regarding their sexual health. Open communication with healthcare professionals remains crucial for effective testing, diagnosis, and treatment.
The subsequent sections will delve deeper into specific STIs, their respective diagnostic methods, and available treatment options.
Tips for Navigating STI Testing and Blood Work
Navigating the complexities of sexually transmitted infection (STI) testing requires awareness and proactive engagement with healthcare services. The following tips offer guidance for informed decision-making and effective management of sexual health.
Tip 1: Understand Individual Risk Factors: Honest self-assessment of sexual behaviors, including number of partners and consistency of protection use, is crucial for determining appropriate testing frequency and the specific STIs for which to be tested. Higher-risk individuals might benefit from more frequent screenings.
Tip 2: Consult Healthcare Professionals: Open communication with healthcare providers regarding sexual history, potential exposures, and any concerning symptoms is essential for accurate risk assessment and tailored testing strategies. Professional guidance ensures appropriate test selection and interpretation of results.
Tip 3: Recognize Testing Limitations: Awareness of the detection window for different STIs and the potential for false negatives and false positives in blood work and other diagnostic tests is crucial for managing expectations and interpreting results accurately. Repeat testing might be necessary, particularly if initial results are negative and suspicion of infection remains.
Tip 4: Adhere to Recommended Testing Timelines: Following recommended testing intervals for specific STIs, based on individual risk factors, maximizes the likelihood of early detection and timely intervention. Regular screening contributes to individual and public health by reducing the risk of onward transmission.
Tip 5: Seek Confirmatory Testing When Necessary: When initial screening tests yield positive or ambiguous results, pursuing confirmatory testing provides a higher level of certainty and informs appropriate treatment decisions. Confirmatory testing minimizes the risk of misdiagnosis and ensures accurate management.
Tip 6: Prioritize Holistic Sexual Health: STI testing is just one component of comprehensive sexual health management. Practicing safer sex, including consistent condom use and open communication with partners, remains crucial for reducing the risk of STIs and other sexual health concerns.
Tip 7: Access Reliable Information Sources: Consulting reputable sources, such as healthcare providers, public health organizations, and evidence-based websites, ensures access to accurate and up-to-date information regarding STI testing, prevention, and treatment.
Adopting these proactive strategies empowers individuals to take control of their sexual health and make informed decisions regarding STI testing and blood work. Regular communication with healthcare providers is essential for effective management and risk mitigation.
The concluding section will summarize key takeaways and offer further resources for continued learning and support.
Understanding STI Detection Through Blood Work
The exploration of whether sexually transmitted infections (STIs) manifest in blood work reveals a complex interplay of factors. The type of STI significantly influences detectability, with infections like HIV and syphilis readily identified through blood tests, while others, like chlamydia and gonorrhea, necessitate specialized tests such as NAATs. The detection window, the period between infection and detectability, varies considerably among STIs, impacting result interpretation. Accuracy variations inherent in testing methodologies, including biological factors and laboratory procedures, underscore the importance of confirmatory testing for reliable diagnoses. False negatives, arising from testing within the window period or utilizing inappropriate tests, pose significant challenges to timely intervention. Understanding these intricacies is crucial for effective STI management.
The accurate and timely detection of STIs remains paramount for individual and public health. Proactive engagement with healthcare professionals, coupled with informed decision-making regarding testing strategies, empowers individuals to protect their well-being and contribute to broader STI control efforts. Continual advancements in diagnostic technologies offer hope for enhanced detection and improved management of these infections in the future. Prioritizing sexual health education and access to reliable testing services remains crucial for mitigating the impact of STIs on global health.



